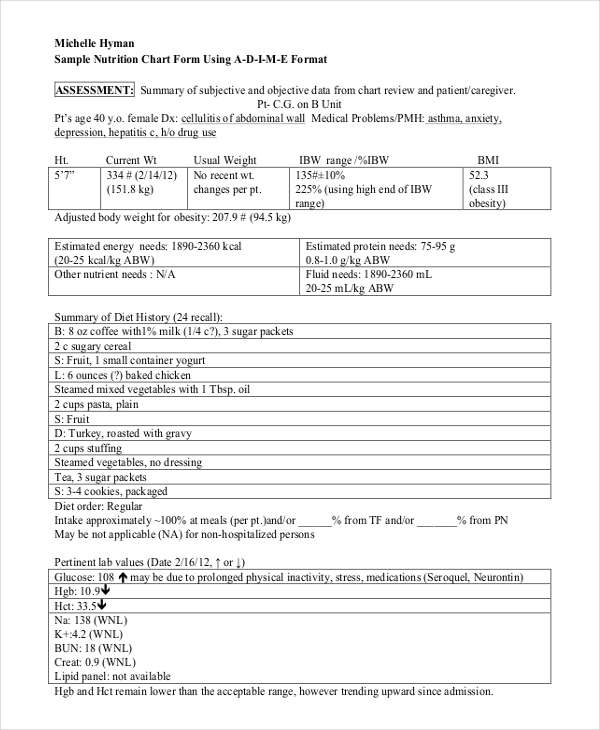
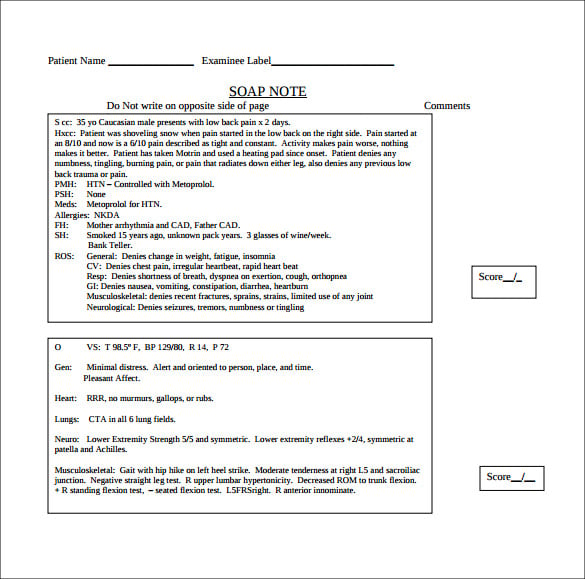
It’s far more important to take accurate notes, including your opinions, than to leave medical charts incomplete. anne w. latner, jd, is a former criminal defense attorney and a freelance. Doctors and health service providers can use this downloadable template to document a patient’s medical details during an appointment, from initial exam to progress notes. this template includes space to detail everything from main medical concerns to reason for visit, family and medical history, and insurance information. Medical chart notesmedical chart notes. s. o. a. p. a chartnote usually follows a very simple pattern: subjective (what the patient thinks) = s objective (what the doctor thinks) = o assessment (what the diagnosis is) = a plan (what happens next) = p. See more videos for medical chart notes.
Medical terminology information sheet.

60 Funny Charting Errors Found On Actual Medical Records
politics doctors flood congress with lobbyists on surprise medical bills 4 hours ago / us news energy ben geman 1 hour ago tesla's hefty electric vehicle market weight reproduced from cox automotive ; note: does not include plug-in hybrids; chart: axios visuals for all the justified worries about Enjoy these funny charting errors and bloopers found on actual medical records! most of the time, work can be stressful and paperwork are piling up like there’s no tomorrow. trying to catch up and finishing charting before the end of the shift you rush and forget everything you’ve learned from your english classes. A soap (subjective, objective, assessment, plan) note is a method of documentation used specifically by healthcare providers. soap notes are used so staff can write down critical information concerning a patient in a clear, organized, and quick way. soap notes, once written, are most commonly found in a patient’s chart or electronic medical records.
How to write progress notes and communicate in medical charts: daniel sexton, m. d. duke university medical center first person active tense is more effective than the passive voice simple declarative sentences are best. •forgetting to place an operative note on the chart the instant after a procedure or operation is performed: –the surgeon may dictate the operative note, but will write a postoperative note so there is documentation on the chart when the patient gets care elsewhere, i. e. recovery room, on the med-surg unit, or at home if discharged. The timing of a medical record note is especially important in inpatient charts, emergency department settings, trauma settings, and critical care units. it’s especially critical for the service provider’s identity to be legible. signatures also should include the provider’s credentials. medicare comment no. 5.

As needed from a referring physician’s office (for example, physician order, notes to medical chart notes support medical. necessity) or from an inpatient facility (for example, progress note). the. medicare program integrity manual, chapter 3, section 3. 2. 3. 3, “third-party additional documentation request” states:. Put time and date on all entries in the medical record. notes should be contemporaneous. label added information as addendum and indicate when it was entered. do not alter existing documentation or withhold elements of a medical record once a claim emerges. periodically a physician defendant fails to heed this age-old advice.
Free Medical Form Templates Smartsheet
A chart note, also called a progress note or office note, is dictated when an established patient is seen for a repeat visit. a chart note records the reason for the current visit, an assessment of the patient’s condition (including any changes since the previous visit), and additional treatment rendered or planned. Guidelines for medical record documentation 2 16. there is review for under or overutilization of consultants. 17. if a consultation is requested, there a note from the consultant in the record. 18. consultation, laboratory and imaging reports filed in the chart are initialed by the practitioner who ordered them, to signify review. Medical chart notes. s. o. a. p. a chart note usually follows a very simple pattern: s ubjective (what the patient thinks) = s. o bjective (what the doctor thinks) = o. a ssessment (what the diagnosis is) = a. p medical chart notes lan (what happens next) = p. not all providers dictate the “soap” note format; sometimes they simply state in a narrative way the same information.
Enlarging medical records to billboard size may catapult a nurse’s simple note into an embarrassing display of observations gone awry. to prevent charting from receiving such scrutiny and giving an inaccurate perception of the care that was actually delivered, the charting guidelines in the sidebar should be followed. Intermittent dizziness. her past medical history is significant for severe arthritis of her knees, osteoporosis and let hip replacement surgery in the mri indicates she had a right lacunar infarct. her lungs are clear and her bp is reported at 134/42 and 139/73 since admission. there is some evidence of orthostatic hypotension. Please see note. shx: is reviewed. please see note. pe: she has a 2-3 cm well-circumscribed hyperemic area with small clear vesicles. bacterial culture is taken. a viral culture is taken. she has no lymph nodes either in her anterior cervical chain, supra or subclavicular or inguinal area. a&p: likely herpetic rash. cultures have been taken. Note: these transcribed medical transcription sample reports and examples are provided by various users and are for reference purpose only. mthelpline does not certify accuracy and quality of sample reports. these transcribed medical transcription sample reports may include some uncommon or unusual formats; this would be due to the preference of the dictating physician.
How to conduct a medical record review ed/ems notes the process of record review begins with the emergency department (ed) notes, or notes from emergency medical services (ems). here, cdi specialists encounter a great deal of clinical evidence for poa conditions, even if not initially documented in the medical record.
Comments In Chart Lead To A Lawsuit Clinical Advisor
Complying With Medical Record Documentation Requirements
Medicalchart organization: • demographics and insurance • flow sheets • physician orders • visit notes • laboratory results • radiology results • consultant notes • other communications types of patient encounter notes: • •history and physical o pe physical exam o physical examination terms: lab laboratory studies o. Software to create patient encounter (soap) notes without transcription. note is printed and immediatedly placed into charts avoiding medical chart notes chart handling. More medical chart notes images. Psychotherapy notes that are separated from the rest of the individual’s medical record and are recorded (in any medium) by a health care provider who is a mental health professional documenting or analyzing the contents of conversation during a private counseling session or a group, joint, or family counseling session.
Always remember that there are other medical professionals who will also view the note or chart. this is to make decisions regarding your patient’s treatment and care. make your handwriting clear and legible. a lot of medical professionals are encouraged to write coherent notes. this will serve as a defense against any form of legal action. • the “soap” note o s = subjective (what the patient tells you) o o = objective (info from pe, labs, radiology) o a = assessment (dx and ddx) o p = plan (treatment, further tests, etc. ) • discharge summary o narrative in format o summarizes the events of a hospital stay o subjective terminology is used. Medicare chart note requirements to be covered by medicare, all applicable medicare statutory and regulatory requirements must be met. medicare requires a physical evaluation of the patient. please provide the pdfs below to your physician for compliant chart note content (medicare does not consider a letter part of the medical record). please fax any medicare compliant chart notes to our office.
One kind of report you will see in medical transcription is a chart note. a chart note, also called a progress note or office note, is dictated when an established patient is seen for a repeat visit. a chart note records the reason for the current visit, an assessment of the patient’s condition (including any coders utilize information contained in a patient's medical record (documentation, chart notes, lab and x-ray reports, nurse notes, etc) to identify the services and treatment rendered by a medical doctor or other healthcare provider that information is